EDI Claims That Include Diagnosis Codes
Insurance companies may require that diagnosis codes be included in their claims. To accommodate this requirement, 12 diagnosis codes are optionally supported on insurance claims for single visits regardless of Current Procedural Terminology (CPT) pointing.
Before walking through how to configure the use of 12 diagnoses, it is important to review the rules about diagnoses pointed at the charge level:
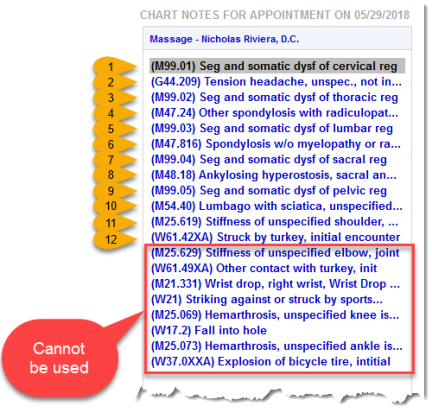
- ChiroTouch allows for inclusion of a maximum of 12 diagnoses per claim, and those diagnoses can only be among the first 12 in the patient's diagnosis list
- A maximum of four (4) diagnoses can be pointed at a single charge
- If no specific diagnoses are selected for a given charge, by default the charge will use the first four on the diagnosis list
To serve as an example, patient Sally Smith has the following diagnoses with the top 12 numbered for illustration:
Looking at the patient's Ledger, the following charges have been logged for the service date of 5/29/2018.
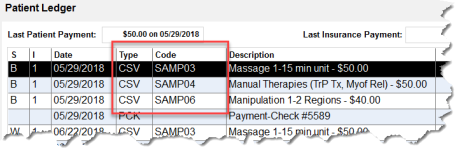
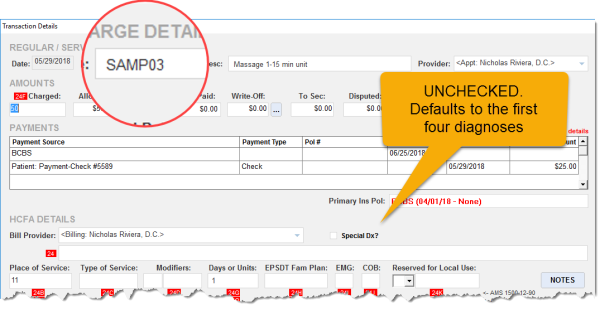
By double-clicking the first charge, Code SAMP03, it can be seen below that "Special Dx?" was not checked. No diagnoses were explicitly pointed to this charge, so the charge defaults to having pointers from diagnoses 1 through 4 from the list:
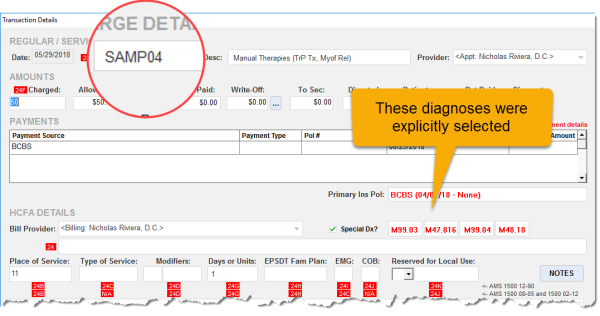
In SAMP04 below, diagnoses 5, 6, 7, and 8 are explicitly pointed at SAMP04:
SAMP06 (not being shown) is similar though its pointers are from diagnoses 3, 4, 7, and 8.
Once the rules about charge-level pointing of diagnoses are understood clearly, you can now enable Diagnosis Codes to appear in insurance claims. Launch CT Accounting and complete the following steps:
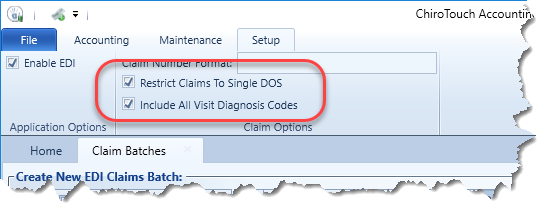
- Click the Setup tab.
- Select the "Restrict Claims to Single DOS" checkbox. (Diagnosis Code inclusion is only enabled for single DOS!)
- Select the "Include All Visit Diagnosis Codes" checkbox:
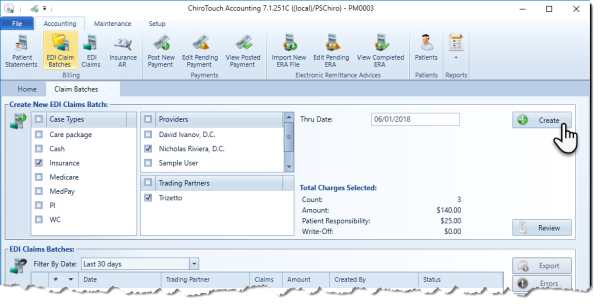
Now you create an EDI Claim Batch, first setting up its parameters as needed. This example covers Insurance cases for Dr. Nick Riviera with a "Thru Date" of 6/1/2018:
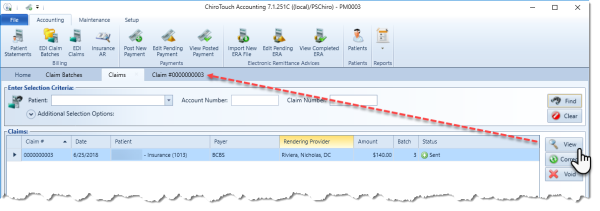
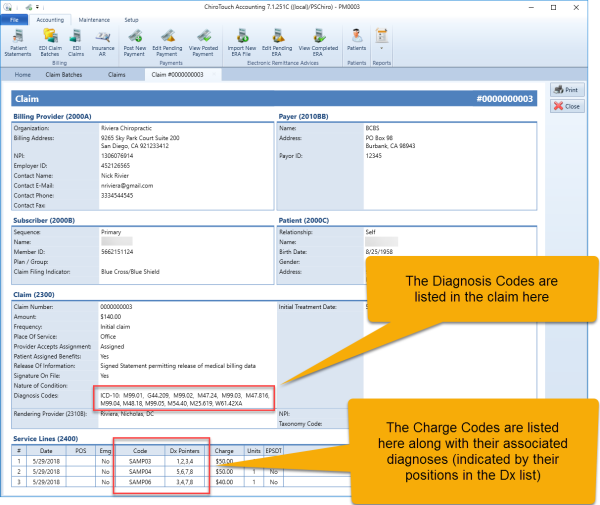
Once the claim is generated, the Diagnosis Code information is viewable. (Note that for simplicity, this Claim Batch contains only one claim):
Remember that ChiroTouch supports charges pointed to the first 12 diagnoses only. Anything beyond 12 will generate an error in CT Accounting.
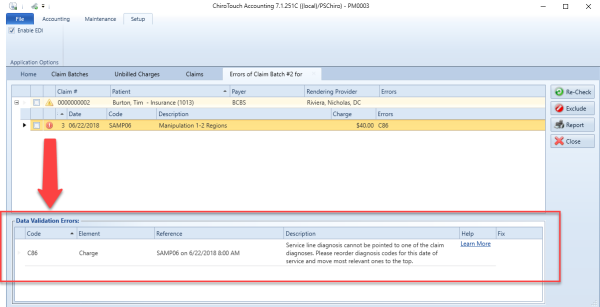
In the example below, a charge from 6/22/2018, the charge has one or more diagnoses pointed outside of the first 12.
Claim Batch error:
If a diagnosis outside of the top 12 is needed, first reorder the list using Provider (Basic) or Provider All-In-One, moving the needed diagnosis up as far as is required to place it within the top 12.
Reordering the diagnosis list: