Health Information Exchange: Sending Health Information – REQUIRED FOR 2024 REPORTING
| Objective name | What that means for you | Is this objective required? |
| Health Information Exchange - Sending Health Information |
For at least one transition of care or referral, the MIPS eligible clinician that transitions or refers their patient to another setting of care or health care provider—(1) creates a summary of care record using certified electronic health record technology (CEHRT); and (2) electronically exchanges the summary of care record. |
Yes, this is a required objective.* |
* Exclusion applied to those who do not refer out of their office more than 100 times during reporting.
Exclusion
Any MIPS eligible clinician who receives transitions of care or referrals or has patient encounters in which the MIPS eligible clinician has never before encountered the patient fewer than 100 times during the performance period.
Reporting Requirements
NUMERATOR/DENOMINATOR
NUMERATOR: The number of transitions of care and referrals in the denominator where a summary of care record was created using CEHRT and exchanged electronically.
DENOMINATOR: The number of transitions of care and referrals during the performance period for which the MIPS eligible clinician was the transferring or referring clinician.
Scoring Information
BASE SCORE/PERFORMANCE SCORE/BONUS SCORE
Required for Promoting Interoperability Performance Category Score: Yes
Measure Score: Up to 20 points
Eligible for Bonus Score: No
Note that MIPS eligible clinicians must:
- Submit a “yes” to the Prevention of Information Blocking Attestations
- Submit a “yes” to the ONC Direct Review Attestation, if applicable
- Submit a “yes” that they have completed the Security Risk Analysis measure during the calendar year in which the MIPS performance period occurs
- Must report the require measures from each of the four objectives in order to earn a score greater than zero for the Promoting Interoperability performance category
Watch this short video to find out about reporting on this measure.
Procedure
You must create a Health Summary using the Task Manager in ChiroTouch and send this summary to the receiving provider via Direct to meet compliance. You can complete this through the Task Manager and Patient Application.
NOTE: If you are referring out of your office less than 100 times during the reporting period you may exclude from this measure and you do not need to subscribe to the Direct Messaging service.
IMPORTANT: You must have the capability to provide a Summary of Care document through your certified technology. This requires Direct Messaging services, if you are not currently subscribed to Direct Messaging you can contact the QPP dept. by opening a case in CTCommunity under CMS Compliance or contact us direct at 619-546-4510 for a quote and more information.
Step I, create a Summary of Care – Referral Summary for your patient through the Task Manager on your Launcher.
Step II, send Summary of Care – Referral Summary to the receiving provider via Direct Messaging through the Patient Application – Referral Summary R2 Information.
Create Summary of Care - Referral Summary R2 Information through the Task Manager:
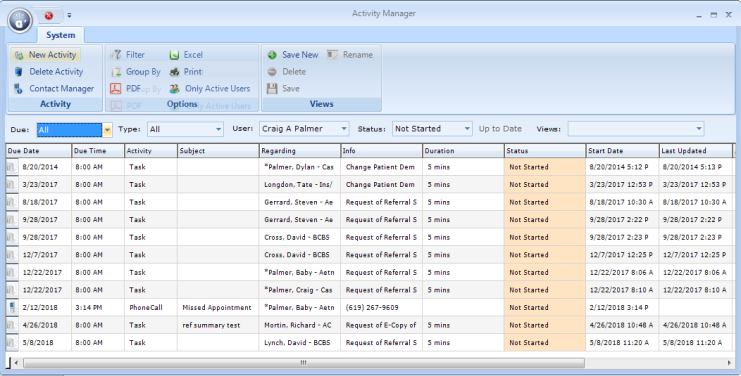
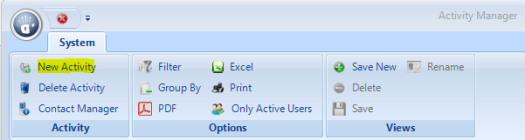
- Open the Activity Manager from the Launcher.
- Click New Activity.
- The software will open the New Activity window. Click Task and click the OK button.
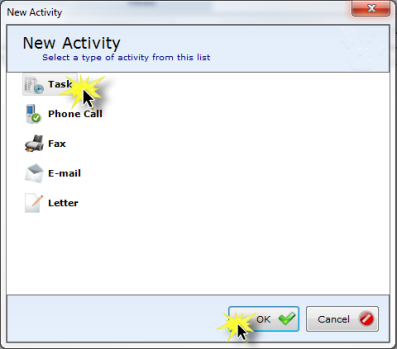
- The software will open the New Task window. Select Request of Referral Summary R2 Information from the Task Type drop-down menu.
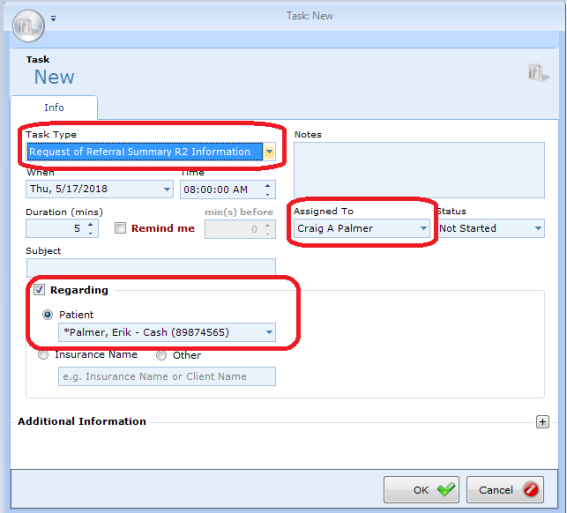
- Update any information necessary for this task (this information will not be reflected on the referral summary) under When, Time, Duration, Subject, Notes, etc.
- To receive compliance the correct provider must be selected under Assigned To.
- Check the box next to Regarding toward the bottom of the window. Once checked you can select the Patient option (if not currently selected) and use the drop-down menu to assign referral to the patient whom you are transitioning or referring to another provider.
- Click OK. On the Task List you should see your most recently created task for referral to the bottom.
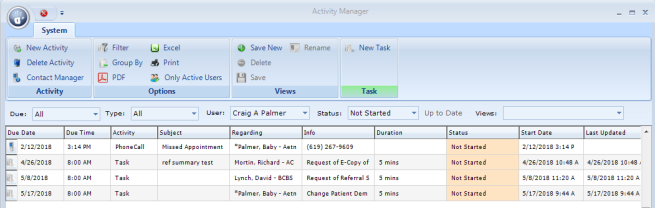
NOTE: If the correct provider is not selected compliance will not be met by this provider and the task will need to be edited to in order to apply this referral summary correctly (You may edit by double-clicking this task from the Task List).
NOTE: Note: If the correct patient is not selected you will not be able to access the summary for this patient and the task will need to be edited to in order to apply this referral summary correctly (You may edit by double-clicking this task from the Task List).
Send Summary of Care – Referral Summary using Direct Messaging to the receiving provider via the Patients application:
- Select the Patients application from your Launcher (if this is not currently present on your Launcher it can be added through Options by right-clicking the hand icon to the top).

- Search for your patient and double-click once the appropriate patient account is visible.
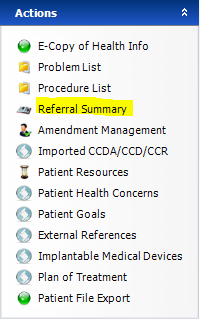
- On the patient Information tab select Referral Summary to the left under Actions.
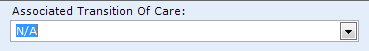
- To the top right of your Referral Summary R2 Document use the dropdown to select the Associated Transition Of Care that you created through the task manager. You will see the creation date to easily access the correct summary.
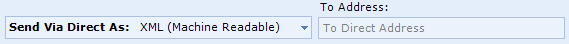
- After selecting the current referral document enter the receiving provider’s Direct email address to the top right under To Address and click Send Via Direct As. (You may choose the format you would like this information to be received with.)
- You will receive a prompt letting you know if your file was sent successfully. You may also choose to send this document to the Patient Portal if requested. Click OK and Close.
- If the file was sent successfully Open your QPP Dashboard and review the Health Information Exchange: Send Summary of Care measure to confirm your compliance.
BEST PRACTICE: Select XML format when transmitting the referral summary to another provider's system. To send a human-readable copy of the referral summary, select PDF (Human Readable) from the Send Via Direct As: drop-down menu.
CRITICAL: You cannot send Protect Health Information (PHI) through a regular email account, like Gmail or Yahoo. This protected information must be encrypted during transmission and accessed on a password protected site or software. You will not be able to achieve compliance when sending any documentation outside of Direct Messaging. If the receiving provider does not have a Direct Messaging service it is the responsibility of the sending provider to locate a compliant recipient for referral.
Transition of Care – The movement of a patient from one setting of care (hospital, ambulatory primary care practice, ambulatory, specialty care practice, long-term care, home health, rehabilitation facility) to another. At a minimum this includes all transitions of care and referrals that are ordered by the MIPS eligible clinician.
Referral – Cases where one provider refers a patient to another, but the referring provider maintains his or her care of the patient as well.
Summary of Care Record – All summary of care documents used to meet this objective must include the following information if the MIPS eligible clinician knows it:
- Patient name
- Demographic information (preferred language, sex, race, ethnicity, date of birth)
- Smoking status
- Current problem list (eligible clinicians may also include historical problems at their discretion)*
- Current medication list*
- Current medication allergy list*
- Laboratory test(s)
- Laboratory value(s)/result(s)
- Vital signs (height, weight, blood pressure, BMI)
- Procedures
- Care team member(s) (including the primary care provider of record and any additional known care team members beyond the referring or transitioning clinician and the receiving clinician)*
- Immunizations
- Unique device identifier(s) for a patient’s implantable device(s)
- Care plan, including goals, health concerns, and assessment and plan of treatment
- Referring or transitioning clinician’s name and office contact information
- Encounter diagnosis
- Functional status, including activities of daily living, cognitive and disability status
- Reason for referral
*Note: A MIPS eligible clinician must verify that the fields for current problem list, current medication list, and current medication allergy list are not blank and include the most recent information known by the MIPS eligible clinician as of the time of generating the summary of care document or include a notation of no current problem, medication and/or medication allergies.
Current problem lists – At a minimum a list of current and active diagnoses.
Active/current medication list – A list of medications that a given patient is currently taking.
Active/current medication allergy list – A list of medications to which a given patient has known allergies.
Allergy – An exaggerated immune response or reaction to substances that are generally not harmful.
Care Plan – The structure used to define the management actions for the various conditions, problems, or issues. A care plan must include at a minimum the following components: problem (the focus of the care plan), goal (the target outcome) and any instructions that the provider has given to the patient. A goal is a defined target or measure to be achieved in the process of patient care (an expected outcome).
MIPS eligible clinicians can report the Promoting Interoperability objectives and measures if they have technology certified to the 2015 Edition, or a combination of technologies from the 2014 and 2015 Editions that support these measures.
In CY 2024, a one-time bonus will be earned by MIPS eligible clinicians and groups who report using 2015 Edition CEHRT exclusively and only submit Promoting Interoperability measures.
This measure contributes to the 50% base score for the Promoting Interoperability performance category. MIPS eligible clinicians must submit a “yes” for the security risk analysis measure, and at least a 1 in the numerator for the numerator/denominator of the remaining measures or claim exclusions. The measure is also worth up to 10 percentage points towards the performance category score. More information about Promoting Interoperability scoring is available on the QPP website.
For the measure, only patients whose records are maintained using CEHRT must be included in the denominator for transitions of care.
In order to count in the numerator, the exchange must occur within the performance period.
A MIPS eligible clinician must have confirmation of receipt or that a query of the summary of care record has occurred in order to count the action in the numerator.
Apart from the three fields noted as required for the summary of care record (i.e., current problem list, current medication list, and current medication allergy list), in circumstances where there is no information available to populate one or more of the fields listed (because the MIPS eligible clinician does not record such information or because there is no information to record), the MIPS eligible clinician may leave the field(s) blank and still meet the measure.
A MIPS eligible clinician must have the ability to transmit all data pertaining to laboratory test results in the summary of care document, but may work with their system developer to establish clinically relevant parameters for the most appropriate results for the given transition or referral. This policy is limited to laboratory test results.
A MIPS eligible clinician who limits the transmission of laboratory test result data in a summary of care document must send the full results upon request (i.e. all lab results as opposed to a subset).
The referring clinician must have reasonable certainty of receipt by the receiving clinician to count the action toward the measure.
The exchange must comply with the privacy and security protocols for ePHI under HIPAA.
In cases where the MIPS eligible clinicians share access to an EHR, a transition or referral may still count toward the measure if the referring provider creates the summary of care document using CEHRT and sends the summary of care document electronically. If a MIPS eligible clinician chooses to include such transitions to clinicians where access to the EHR is shared, they must do so universally for all patient and all transitions or referrals.
The initiating MIPS eligible clinician must send a C–CDA document that the receiving clinician would be capable of electronically incorporating as a C–CDA on the receiving end. If the sending MIPS eligible clinician converts the file to a format the receiving clinician could not electronically receive and incorporate as a C–CDA, the initiating clinician may not count the transition in their numerator.
With the 2015 Edition, we do not intend to continue the policy of allowing a third party to convert the summary of care record transmission to fax as it does not drive toward the overall goal of sending, receiving, or retrieving an electronic summary of care document for this objective.
The Send a Summary of Care measure remains a required measure for the base score in the Promoting Interoperability performance category. For required measures in the base score, CMS requires a one in the numerator or a “yes” response to yes/no measures or claim exclusions. Measures included in the base score are required in order for a MIPS eligible clinician to earn any score in the Promoting Interoperability performance category.
MIPS eligible clinicians may claim the exclusions if they are reporting as a group. However, the group must meet the requirements of the exclusion as a group.
When MIPS eligible clinicians choose to report as a group, data should be aggregated for all MIPS eligible clinicians under one Taxpayer Identification Number (TIN). This includes those MIPS eligible clinicians who may qualify for reweighting such as a significant hardship exception, hospital or ASC-based status, or in a specialty which is not required to report data to the Promoting Interoperability performance category. If these MIPS eligible clinicians choose to report as part of a group practice, they will be scored on the Promoting Interoperability performance category like all other MIPS eligible clinicians.