Health Information Exchange: Receiving and Incorporating Health Information – REQUIRED FOR 2024 REPORTING
| Objective name | What that means for you | Is this objective required? |
| Health Information Exchange - Receiving and Incorporating Health Information |
For at least one electronic summary of care record received for patient encounters during the performance period for which a MIPS eligible clinician was the receiving party of a transition of care or referral, or for patient encounters during the performance period in which the MIPS eligible clinician has never before encountered the patient, the MIPS eligible clinician conducts clinical information reconciliation for medication, medication allergy, and current problem list. |
Yes, this is a required objective.* |
* Exclusion applied to those who do not take on more than 100 referrals during reporting.
Exclusion
Any MIPS eligible clinician who receives transitions of care or referrals or has patient encounters in which the MIPS eligible clinician has never before encountered the patient fewer than 100 times during the performance period.
Reporting Requirements
NUMERATOR/DENOMINATOR
NUMERATOR: The number of patient encounters in the denominator where an electronic summary of care record received is incorporated by the clinician into the certified electronic health record technology (CEHRT).
DENOMINATOR: The number of patient encounters during the performance period for which a MIPS eligible clinician was the receiving party of a transition or referral or has never before encountered the patient and for which an electronic summary of care record is available.
Scoring Information
BASE SCORE/PERFORMANCE SCORE/BONUS SCORE
- Required for Promoting Interoperability Performance Category Score : Yes
- Measuring Score: Up to 20 points
- Eligible for Bonus Score: No
Watch this short video to find out about reporting on this measure.
Procedure
You must receive a Health Summary via Direct Messaging to meet compliance. You can verify that this was received through the Message Center on your launcher.
NOTE: If you are taking on less than 100 referrals during the reporting period you may exclude from this measure and you do not need to subscribe to the Direct Messaging service.
IMPORTANT: You must have the capability to receive a Summary of Care document through your certified technology. This requires Direct Messaging services, if you are not currently subscribed to Direct Messaging you can contact the QPP dept. by opening a case in CTCommunity under CMS Compliance or contact us direct at 619-546-4510 for a quote and more information.
Step I, for patients referred into your care complete compliance by requesting a Summary of Care – Referral Summary from the referring provider (if one has not already been provided via Direct). At this point you will need to inquire if they have a Direct Messaging account and give them your Direct email address.
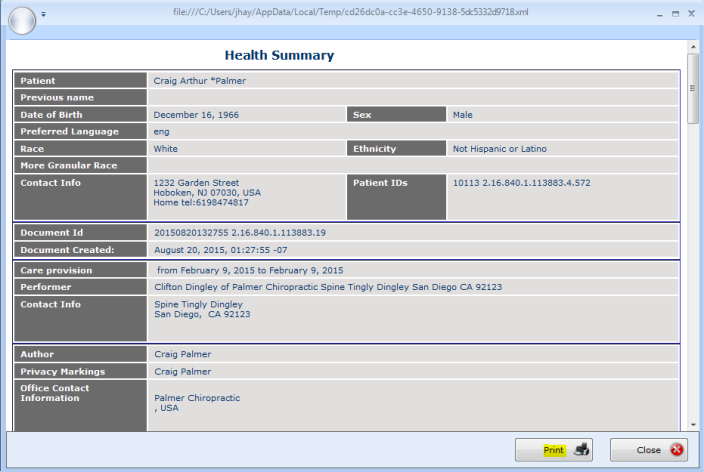
Step II, once this summary is received you can view it through your Messaging Center (and choose to print if necessary). After verifying that the summary was received check your dashboard to confirm your compliance.
Request Summary of Care and supply the referring provider with your Direct address found on the CT Services page on www.mychirotouch.com (skip to step II if referral doc has already been received):

- Log into your www.mychirotouch.com account. The simplest way to achieve this is to access the MyChiroTouch icon from your launcher under the CT Services tab. (Using this link while logged onto your ChiroTouch system will automatically launch you to that site while bypassing the need to enter username or password.)
- From MyChiroTouch.com, click the yellow Services option to the top of the page.

- Scroll down on this page to locate and click your Direct Messaging service information. Click the icon to access Direct Account Information.

- On this page you will find your CT/MaxMD Direct User Email address.
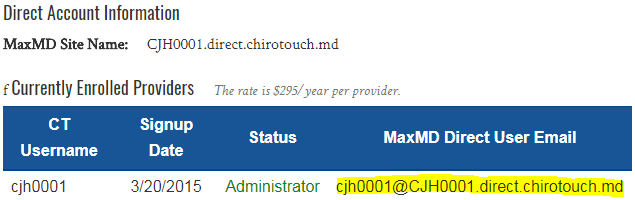
- Give this address to the referring provider to securely transmit the patient health summary from their system into ChiroTouch (this provider must have a Direct Messaging account).
- Once the provider has sent a Summary of Care - Referral document using their Direct emailing service you can find it in your Message Center from the launcher.
NOTE: Note: Direct Messaging is a universal service that can be used with any software regardless of the Direct vendor. If the provider is subscribed they will be aware of the reference to Direct email.
Verify that the summary was received using the Direct Messages tab in the Message Center found on your launcher:
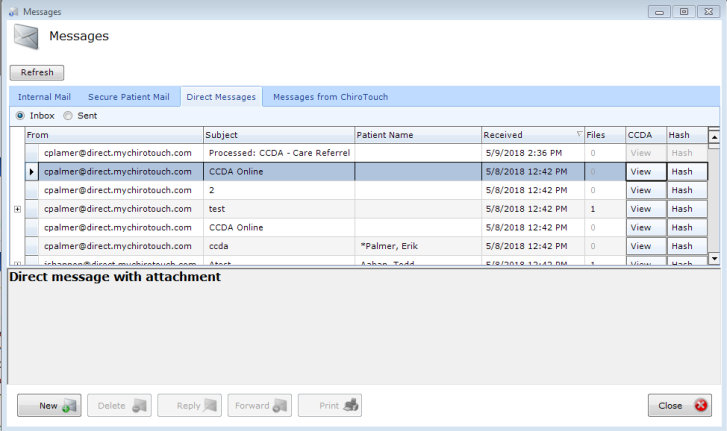
- Access the Message Center from the top of your Launcher.

- Click the Messages option.

- From Messages select the Direct Messages tab.

- On the Direct Messages tab under Inbox review your recently received messages to verify that the referral summary was received.
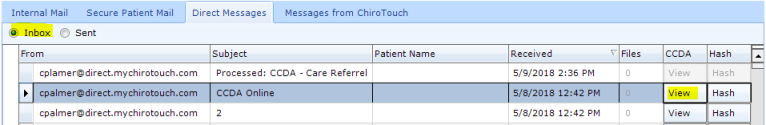
- You may choose to view the document and Print if preferred.
- Open your QPP Dashboard and review the Health Information Exchange: Request/Accept measure to confirm your compliance.
Transition of Care – The movement of a patient from one setting of care (hospital, ambulatory primary care practice, ambulatory, specialty care practice, long-term care, home health, rehabilitation facility) to another. At a minimum this includes all transitions of care and referrals that are ordered by the EP.
- MIPS eligible clinicians can report the Promoting Interoperability objectives and measures if they have technology certified to the 2015 Edition, or a combination of technologies from the 2014 and 2015 Editions that support these measures.
- In CY 2024, a one-time bonus will be earned by MIPS eligible clinicians and groups who report using 2015 Edition CEHRT exclusively.
- Actions included in the numerator must occur within the performance period.
- This measure contributes to the 50% base score for the Promoting Interoperability performance category. MIPS eligible clinicians must submit a “yes” for the security risk analysis measure, and at least a 1 in the numerator for the numerator/denominator of the remaining measures or claim exclusions. The measure is also worth up to 10 percentage points towards the performance category score. More information about Promoting Interoperability scoring is available on the QPP website.
- For the purposes of defining the cases in the denominator for the measure, we stated that what constitutes ‘‘unavailable’’ and, therefore, may be excluded from the denominator, will be that a MIPS eligible clinician— o Requested an electronic summary of care record to be sent and did not receive an electronic summary of care document; and
- The MIPS eligible clinician either:
- Queried at least one external source via health information exchange (HIE) functionality and did not locate a summary of care for the patient, or the clinician does not have access to HIE functionality to support such a query.
or: - Confirmed that HIE functionality supporting query for summary of care documents was not operational in the provider’s geographic region and not available within the MIPS eligible clinician’s EHR network as of the start of the performance period.
- Queried at least one external source via health information exchange (HIE) functionality and did not locate a summary of care for the patient, or the clinician does not have access to HIE functionality to support such a query.
- The MIPS eligible clinician either:
- For the measure, a record cannot be considered to be incorporated if it is discarded without the reconciliation of clinical information or if it is stored in a manner that is not accessible for MIPS eligible clinician use within the EHR.
- The Request/Accept Summary of Care measure remains a required measure for the base score in the Promoting Interoperability performance category. For required measures in the base score, CMS requires a one in the numerator or a “yes” response to yes/no measures or the claiming of exclusions. Measures included in the base score are required in order for a MIPS eligible clinician to earn any score in the Promoting Interoperability performance category.
- MIPS eligible clinician may claim the exclusions if they are reporting as a group. However, the group must meet the requirements of the exclusion as a group.
- When MIPS eligible clinicians choose to report as a group, data should be aggregated for all MIPS eligible clinicians under one Taxpayer Identification Number (TIN). This includes those MIPS eligible clinicians who may qualify for reweighting such as a significant hardship exception, hospital or ASC-based status, or in a specialty which is not required to report data to the Promoting Interoperability performance category. If these MIPS eligible clinicians choose to report as a part of a group practice, they will be scored on the Promoting Interoperability performance category like all other MIPS eligible clinicians.