What Is Quality Reporting?
Quality reporting is one category of the new Quality Payment Program and its sub-program, Merit Based Incentive Payment Program (MIPS). The name Quality derives from the concept of patients' quality-of-care. It generally consists of patient treatment and outcome information.
You can report Quality data to The Centers for Medicare and Medicaid (CMS) in much the same way that you reported PQRS (from 2011-2016), using G-Coded claims (see note below). Or, you may choose to report Quality information through Clinical Quality Measures or CQMs, a method available through the Quality Center and the QPP Dashboard.
IMPORTANT: Quality reporting is required for the full year. All individuals and groups of 15 members or less can use both claims and/or CQM submission methods. CMS will accept non-duplicative measures from both methods.
G-Coded Claims
Reporting Quality information by way of G-coded claims is described here. Once you are set up to do so, your reporting occurs every time you file a Medicare claim.
Clinical Quality Measures
Reporting Quality information though CQMs consists of assessing your patient’s healthcare and lifestyle choices and intervening where appropriate. When a patient treated during the reporting period falls within a certain demographic, and the appropriate diagnosis for the visit is added—or a particular diagnosis is used, a denominator is created. Once the required action is taken for that patient relating to the demographic or diagnosis, a numerator is created in return. This completes your Quality Compliance for that patient.
Generally, you would strive to place over 20 patients in the denominator and complete this compliance (generating a numerator) for these 20 or more, as this is the required minimum for scoring these measures. However if this not possible due to your scope of practice, CMS will score you on any cases submitted once their measures validation is completed.
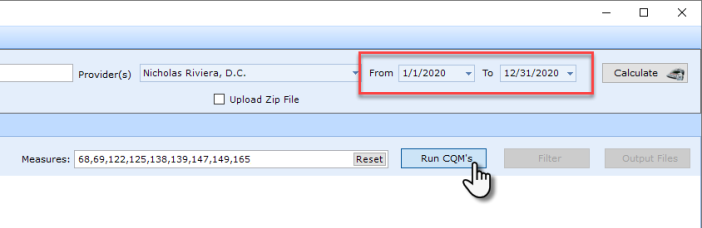
When running the CQMs Report, ensure that the date range in the QPP Dashboard set for the entire year. For example:
What if You Report Both G-Coded Claims and CQMs?
If as a participating provider you submit data using both the G-Code and Clinical Quality Measure reporting options, CMS will apply the higher scoring submission for each measure to your Composite Performance Score.